Abstract
Introduction: Despite the rapidly evolving therapeutic landscape for relapsed or refractory (R/R) diffuse large B-cell lymphoma (DLBCL), treatment with chemotherapy, single-agent rituximab/obinutuzumab, single-agent lenalidomide, or combinations of these agents are common components of R/R DLBCL treatment regimens. This study aimed to characterize clinical outcomes in a real-world cohort of patients with R/R DLBCL treated with the above SOC regimens in the second-line or later setting and to assess the impact of patient demographics and clinical characteristics on clinical outcomes.
Methods: This retrospective, observational study used data from the COTA electronic health records database (COTA, New York, NY). The study included adults diagnosed with DLBCL between January 1, 2010, and March 31, 2022, treated with ≥ 1 prior systemic line of therapy (LOT), including ≥ 1 anti-CD20 monoclonal antibody-containing regimen. Patients had an evaluable response assessment for these R/R DLBCL treatment regimens: chemotherapy, single-agent rituximab/obinutuzumab, single-agent lenalidomide, or combinations of these agents. Treatment outcomes were evaluated using real-world overall response rate (rwORR), real-world complete response (rwCR) rate, real-world duration of response (rwDOR), real-world duration of complete response (rwDOCR) rate, real-world progression-free survival (rwPFS), and overall survival. Subgroup analyses were conducted for patients with ≥ 2 prior LOTs. Logistic regression and Cox proportional hazards regression analyses evaluated the association between outcomes and patient demographics and clinical characteristics.
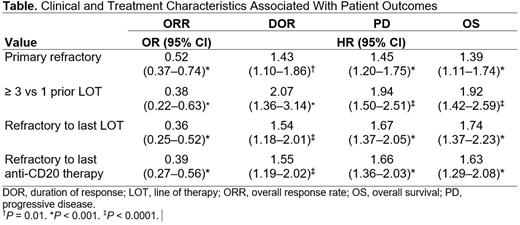
Results: Overall, 573 patients with R/R DLBCL who had ≥ 1 prior LOT were included in the study; of these, 179 patients (31.2%) had ≥ 2 prior LOTs. Median duration of follow-up was 7.7 months. More than one-half (57.1%) were men; 49.9% were aged > 65 years (aged > 75 years, 20.8%) at diagnosis; 82.0% had an ECOG performance status of 0 to 1; 2.8% had prior exposure to chimeric antigen receptor T-cell (CAR T) therapy; 7.0% had prior autologous stem cell transplant; 62.0% had primary refractory disease; 68.6% were refractory to their last LOT; and 67.7% were refractory to their most recent anti-CD20 therapy. Patients experienced worsening outcomes as they progressed through LOTs. In patients with ≥ 1 prior LOT, rwORR was 52% (95% CI: 48-56), rwCR rate was 23% (95% CI: 19-27), median rwPFS was 3.0 (95% CI: 2.8-3.3) months, and median overall survival (mOS) was 12.9 (95% CI: 10.1-16.9) months. In the subgroup with ≥ 2 prior LOTs, rwORR was 40% (95% CI: 33-48), rwCR rate was 13% (95% CI: 8-19), median rwPFS was 2.4 (95% CI: 2.0-2.7) months, and mOS was 6.2 (95% CI: 5.2-10.9) months. In patients with ≥ 3 prior LOTs, rwORR was 34% (95% CI: 23-45), rwCR rate was 8% (95% CI: 3-16), rwDOR was 2.3 (95% CI: 1.3-3.3) months, rwDOCR was 8.5 (95% CI: 2.1-not estimable) months, median rwPFS was 1.9 (95% CI: 1.5-2.5) months, and mOS was 5.1 (95% CI: 3.2-7.3) months. Factors consistently associated with worse efficacy outcomes were primary refractory disease, refractory to last LOT, and refractory to last anti-CD20 therapy (Table). These characteristics indicated elements of a patient population with difficult-to-treat R/R DLBCL, with a 48%-66% lower likelihood of achieving a rwORR; a 45%-101% higher risk of progression; and a 39%-111% higher risk of mortality than those without these characteristics.
Discussion: Patients with R/R DLBCL who received an increasing number of prior LOTs, had primary refractory disease, were refractory to their last LOT, were refractory to their last anti-CD20 therapy, or had prior exposure to CAR T therapy had poor outcomes, with an rwORR (rwCR rate) of 40% (13%) and 34% (8%) in patients with ≥ 2 prior LOTs and ≥ 3 prior LOTs, respectively. This is consistent with prior retrospective analyses of pretreated DLBCL (Crump et al, Blood 2017; Hamadani et al, Clin Lymphoma Myeloma Leuk 2022).
Conclusions: Outcomes in patients with R/R DLBCL treated with chemotherapy, single-agent rituximab/obinutuzumab, single-agent lenalidomide, or combinations of these agents remain poor, especially those with difficult-to-treat R/R DLBCL. These findings underscore the high unmet need for new, safe, and effective therapies across this population, including the difficult-to-treat R/R DLBCL subgroups.
Disclosures
Ip:TG Therapeutics: Membership on an entity's Board of Directors or advisory committees; AstraZeneca: Membership on an entity's Board of Directors or advisory committees; SecuraBio: Membership on an entity's Board of Directors or advisory committees; Seagen: Speakers Bureau; Pfizer: Honoraria. Mutebi:Genmab: Current Employment, Current equity holder in publicly-traded company. Wang:Genmab: Current Employment, Current equity holder in publicly-traded company. Jun:Genmab: Current Employment, Current equity holder in publicly-traded company. Kalsekar:Genmab: Current Employment, Current equity holder in publicly-traded company. Rivas Navarro:Genmab: Current Employment, Current equity holder in publicly-traded company. Wang:AbbVie: Current Employment, Current equity holder in publicly-traded company. Kamalakar:AbbVie: Current Employment, Current equity holder in publicly-traded company. Sacchi:Genmab: Current Employment, Current equity holder in publicly-traded company. Elliott:Genmab: Current Employment, Current equity holder in publicly-traded company.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal